Anatomy
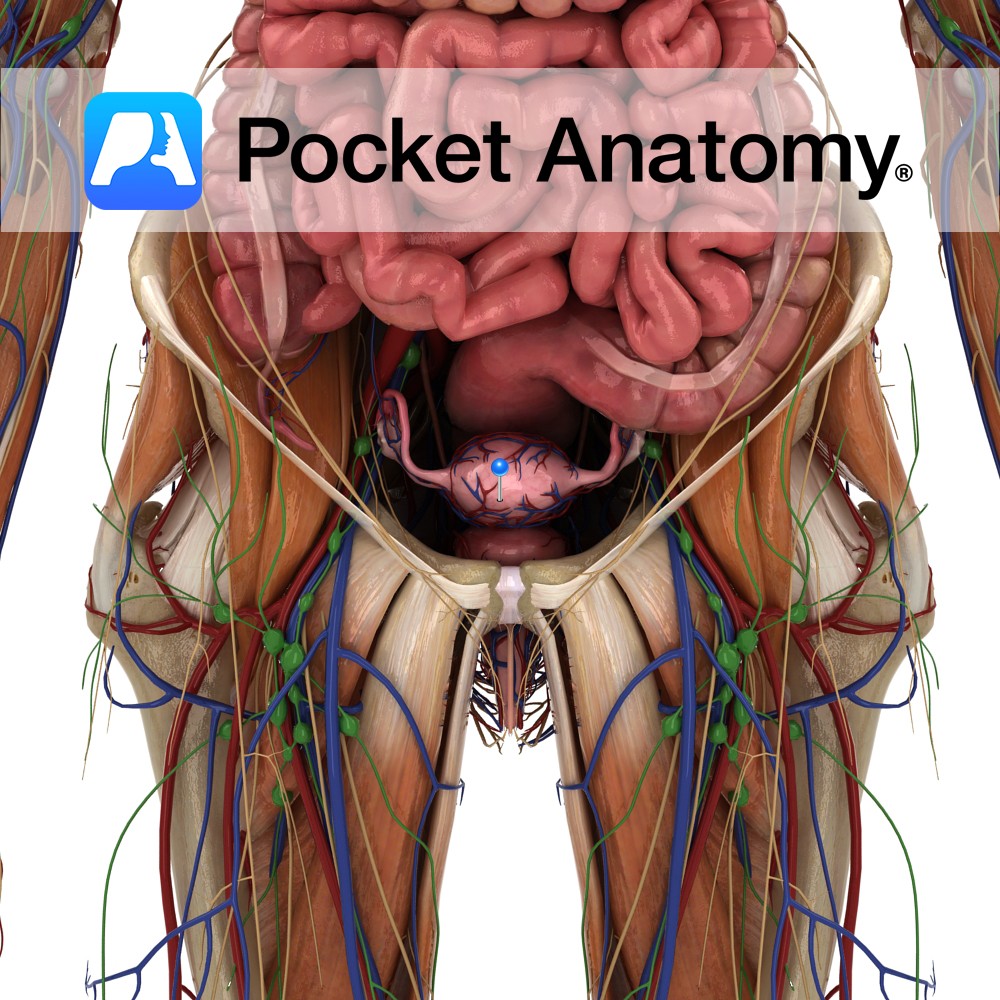
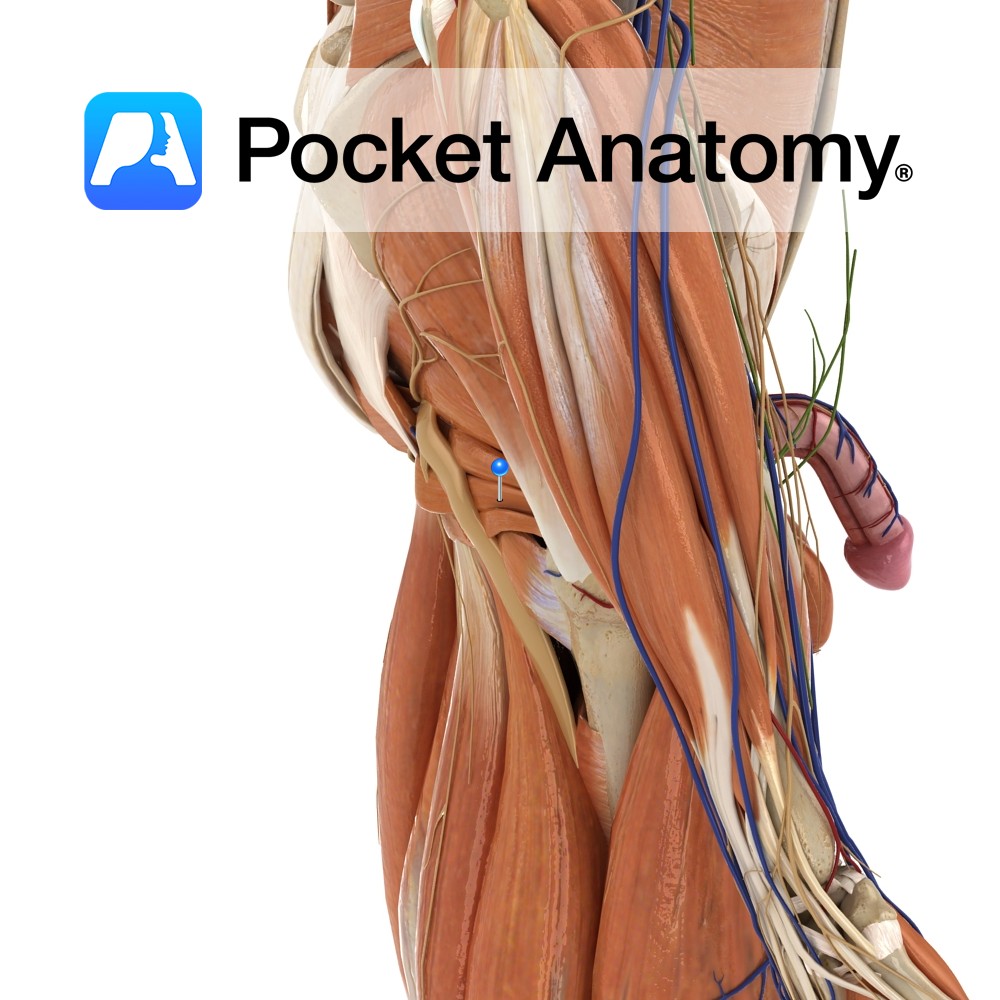
Hollow thick-walled pear-shaped muscular pelvic (and also abdominal when gravid/pregnant) reproductive organ, approximately 7cms long X 5 wide when non-gravid/empty. Body (upper 2/3 of uterus/womb) rounded at top (fundus) where it is joined at the side/cornu/horn by fallopian tubes, uterine cavity narrows at bottom of body (isthmus) at beginning of cylindrical neck/cervix (lower 1/3) which has supra-vaginal and infra-/intra-vaginal parts and internal/external os with intervening/connecting canal, opening into vagina below.
Blanketed/covered from above and sides by peritoneum (attached to pelvic walls) which in folding/tucking around its top and sides (lower cervix projects into vagina and is not covered) forms a double fold within which vessels and ligaments (some of which are local thickenings of these folds) course. Peritoneal covering also forms gutters/pouches between uterus and bladder in front (uterovesical pouch- usually empty) and uterus and rectum behind (rectouterine pouch). Held in place by pelvic floor (particularly the levators ani) and fascia (particularly attaching to cervix) and by several ligaments.
The convex top of the uterus (uterus is body and neck; body is fundus and cavity; neck/cervix is internal os, endocervical canal, external os). Covered by peritoneum/perimetrium, on which coils of small intestine ordinarily sit. Behind and below pubic symphysis in non-pregnant state, rising to xiphisternum in late pregnancy.
Uterine Cavity: Triangular-shaped uterine lumen/space/cavity (in non-gravid/-pregnant state), flattened front-to-back, corners of base above being the fallopian tube os either side, apex below being internal os cervix.
Myometrium: Middle of 3 layers of wall of uterus (endo-, myo-, peri-metrium), muscular (smooth/involuntary).
Endometrium: Mucous/glandular (mucus noun, mucous adjective) membrane, innermost of 3 layers of wall of uterus/womb (endo-, myo-, peri-metrium), builds up monthly (roughly 28-day cycle – 21 building/proliferating, 7 shedding) under influence of estrogen, in anticipation of arrival and implantation of blastocyst (fertilised egg), sheds (some resorption) as menstrual bleeding/period or forms placenta (made of both maternal and fetal cells) to support growing fetus.
Physiology
Under powerful hormonal control (mainly estrogen and progesterone), prepares (and “stands down” or sheds) its internal lining (endometrium) each month – from menarche to menopause – for reception/implantation/nurturing of blastocyst/embryo/fetus/baby, expands greatly as gestation progresses over 40/52, extrudes/passes/delivers baby and placenta/afterbirth through process of labour (involving contraction of the myometrium). Allows passage of sperm up from external os of cervix to the proximal ostium of fallopian tube.
During pregnancy, myometrial cells proliferate and stretch to accommodate growing baby (wall thins). During labour, there is co-ordinated contraction, which exerts pressure on cervix and vaginal wall, which feeds back to hypothalamus and in turn causes release of oxytocin, which feeds back positively to cause further contractions (Ferguson reflex), until baby born, at which point further contraction delivers placenta and squeezes vessels to minimise blood loss.
Endometrium proliferates/builds under influence of estrogen, becomes rich in blood vessels. At ovulation, ovary produces progesterone which redirects endometrium to secretory role. Secretions help blastocyst to land/attach, vessel-richness helps take root/implant.
Clinical
In pregnancy, the volume of the uterine cavity can increase 1000-fold, from around 10mls to 10 litres.
Also, in pregnancy, the “height” (ie upward extent) of the fundus can be assessed clinically by palpation/feeling the abdominal wall, and using the landmarks of pubic symphysis, navel (umbilicus) and bottom of breastbone (xiphisternum), the stage of fetal growth and gestation (how long pregnant) can be estimated (ultrasound more accurate). Roughly; 16/52- 3 finger-widths above symphysis, 20 – 3 below umbilicus, 24 – umbilicus, 28 – 3 above umbilicus, 32 – halfway umbilicus-xiphisternum, 36 – xiphisternum, 40 – 2 fingers lower (as baby’s head moves down, ready for birth).
Placenta at full term (ie 40 weeks) is disc-like organ (about 4-5″ radius, 1-2 lb weight), formed of both fetal and maternal cells, attached to inner wall of womb and by umbilical cord to baby, filters baby waste out and nutrients in and performs gas exchange, provides antibodies from mother which act as “passive immunity” for fetus and newborn, forms barrier to protect fetus from maternal microbes, acts as go-between for maternal and baby circulatory systems, secretes hormones including HCG (presence detected in urine in pregnancy test), shed/discarded after birth/parturition (as “afterbirth”) of baby. Unique, disposable, single-use organ composed of cells of two individuals.
Fibroids are common benign tumours of myometrial cells, commonest in later reproductive life. Usually asymptomatic though can cause heavy/painful periods (menorrhagia/dysmenorrhea), painful intercourse (dyspareunia), urinary/defecation symptoms, backache, abdominal pain, infertility/miscarriage (rarely). Can be subserosal (under/beside perimetrium), intramural (within myometrium), submucosal (beside/under endometrium), pedunculated (on a stalk, projecting into uterine cavity). Shrink after menopause. Treatment, when necessary, includes symptomatic medication, surgery – including hysterectomy, ultrasonic/radiofrequency ablation.
Interested in taking our award-winning Pocket Anatomy app for a test drive?


.jpg)
.jpg)