Anatomy
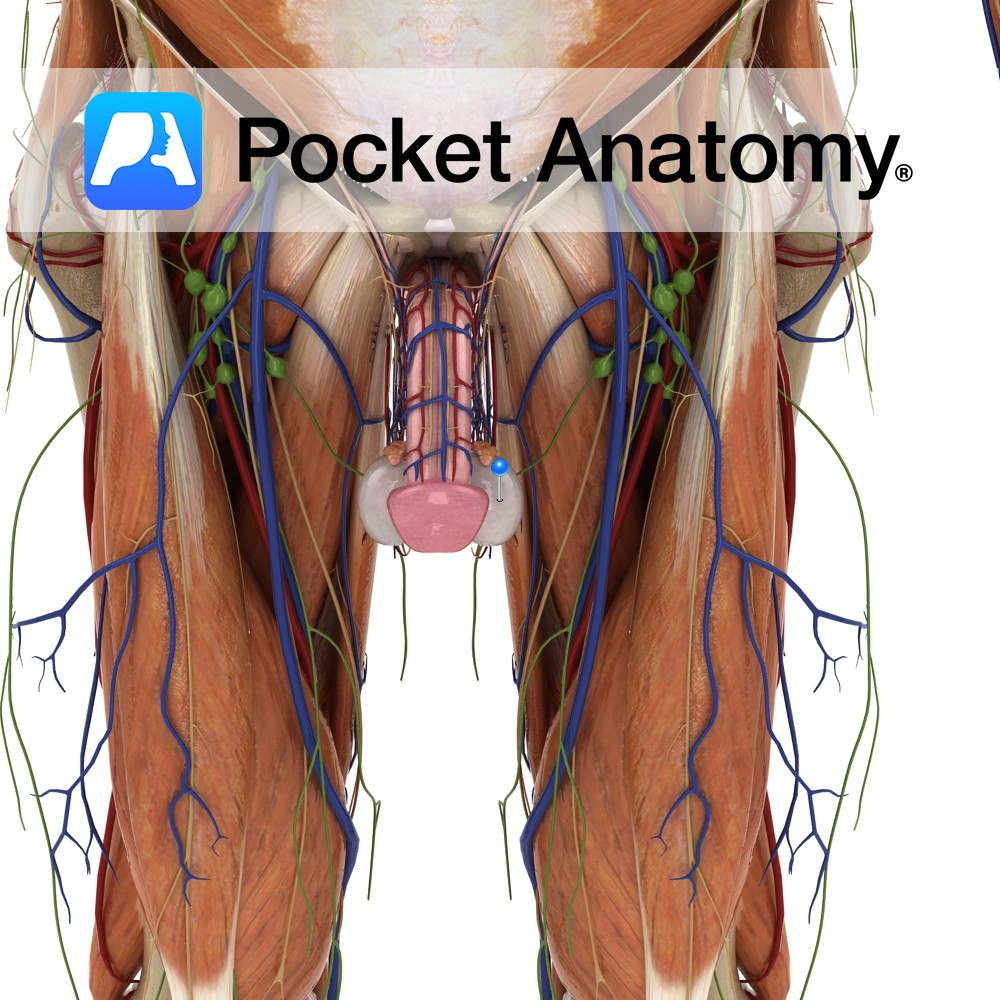
Male gonad [organ that makes gametes – sperm – through a process (spermatogenesis) that involves a type of cell division (meiosis) that produces cells that are haploid, ie have half the chromosome complement of other – diploid – cells; female gamete is ovary, its meiotic product are eggs], produces sperm and testosterone, ellipsoid (about 5x3x2cms, 12-30cc, 25gm).
It is also a gland (makes and releases a substance) both exocrine (produces substance – sperm – and extrudes it through ducts) and endocrine (produces hormones – androgens, mainly testosterone – and secretes them directly/ductlessly into bloodstream), sits in pouch in scrotum, derived from and connected to abdomen by spermatic cord and cremaster muscle, made up of 200-400 wedge-shaped lobes (converging on mediastinum/hilum at back/rear or anal aspect) each with 3-10 seminiferous tubules which have stem cells that produce sperm cells (spermatogenesis) with support of Sertoli cells and under influence of androgen hormones (mainly testosterone from Leydig cells).
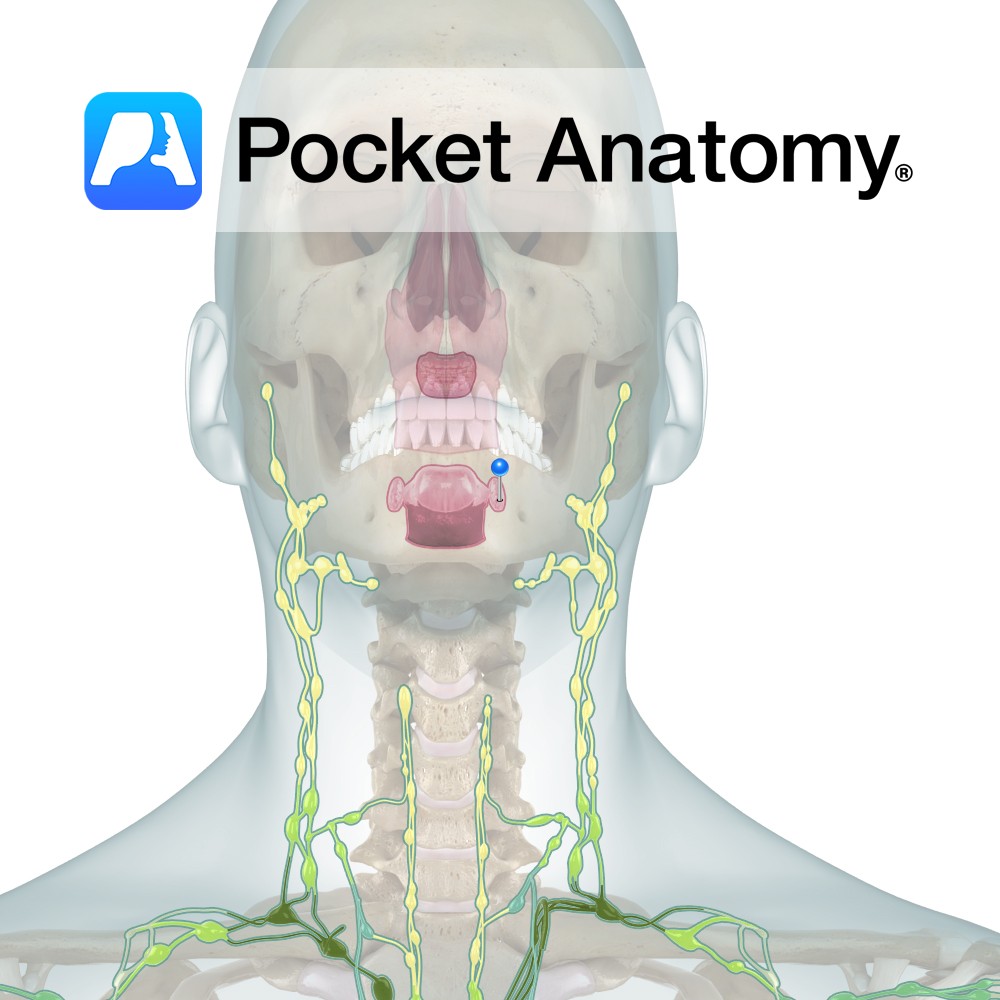
It is supplied by testicular artery via abdominal aorta with collateral supply from cremasteric artery via inferior epigastric via external iliac and vas deferens artery via inferior vesical via internal iliac, lymphatic drainage to para-aortic nodes (and of scrotum to inguinal nodes).
Seminiferous Tubule: There are 3-10 seminiferous tubules in each of 200-400 lobules of testis (testis invested in tunica albuginea, lobules separated by septa). There is interstitial tissue (with endocrine Leydig cells) between tubules. Tubules are the location of spermatogenesis (exocrine). The seminiferous tubules have a basement membrane on which sit type A spermatagonia (stem cells which continue to proliferate – mitosis – through life, with some progeny undergoing meiosis) and Sertoli cells (a set number/population from once spermatogenesis begins after about age 1).
Spermatagonia, which undergo meiosis, graduate away from basement membrane towards tubule lumen, such that the stratified epithelium of the tubule is made up (BM to lumen) of progressively developing sperm cells.
Type A spermatagonia divide by mitosis to form intermediate spermatagonium. Intermediate spermatagonium divide again, some to become and replenish the stock of type A spermatagonia, others to become type B spermatagonium.
Type B spermatagonium divide to become primary spermatocytes, which divide through meiosis (I) to become secondary spermatocytes.
Secondary spermatocytes quickly divide by meiosis II to become spermatids (mitosis – diploid to diploid, ie 46 chromosomes to 46; meiosis – diploid to 2 X haploid, ie 46 to 2 X 23). Spermatids mature to spermatozoa, which are released into the lumen of the seminiferous tubule to begin a long journey. Spermatogenesis begins at the basement membrane of the tubule epithelium, each subsequent phase bringing the developing sperm closer to the tubule lumen.
Sertoli cells nurture cells undergoing spermatogenesis, move them progressively towards the lumen, protect them from immune response (tight junctions between sertoli cells constitute blood-testis barrier, forming basal and adluminal compartments).
Vas Deferens: Muscular 12-18″ excretory duct of testis, one of the spermatic cord structures, connecting epididymis (in the scrotum) to the ejaculatory duct (1″) in pelvis, which is formed by union of vas and duct of seminal vesicle (vas passes up and over the top of the bladder and down behind it, ending just medial to lower end of ureters, at level of pubic symphysis).
Physiology
Vas propels sperm by peristalsis during ejaculation.
Clinical
Vasectomy is a relatively straightforward, low-risk, effective (<1% failure rate) form of permanent (though surgical reversal may be possible) male contraception, carried out under local anaesthesia.
Interested in taking our award-winning Pocket Anatomy app for a test drive?


.jpg)